Our Focus
Healthcare-Associated Infections (HAIs), Biofilms and High Touch Surfaces
Healthcare-associated infections (HAIs) are infections patients develop while receiving medical treatment. In the United States, they affect roughly 1.7 million patients each year and contribute to about 99,000 deaths. These infections—caused by bacteria, viruses, fungi, or other pathogens—are also expensive, with some of the most common HAIs costing over $40,000 per individual case.
Pathogens can survive on hospital surfaces despite rigorous cleaning, exposing patients through contact with the environment, healthcare workers, or their own skin. On any given day, 1 in 31 hospitalized patients has at least one HAI.
The growing threat of multi-drug resistant organisms (MDROs), driven in part by antibiotic overuse, further complicates prevention efforts. Overall, this increases the need for more comprehensive disinfection practices.
Common types of HAIs include:
CLABSI: Central line–associated bloodstream infections
CAUTI: Catheter-associated urinary tract infections
SSI: Surgical site infections
VAP: Ventilator-associated pneumonia
HAIs impose a significant financial burden, costing the U.S. healthcare sytem an estimated $28–45 billion annually. They continue to be a major patient safety challenge.
Yet prevention is highly effective. Facilities that adopt targeted infection-prevention practices—such as proper central line and catheter care, minimizing unnecessary catheter use, strong antibiotic stewardship, and close coordination with surgical teams—can reduce some HAIs, e.g. CLABSIs and CAUTIs.
By strengthening environmental hygiene, ensuring meticulous patient care, and improving antibiotic use, healthcare institutions can substantially reduce HAIs, save lives, and lower healthcare costs.
Biofilms in Medicine and Everyday Life
Biofilms are communities of microorganisms that form following the attachment of planktonic (free-floating) bacteria to surfaces. With proper nutrition, cell replication and creation of a protective cellular polymeric substance (biofilm) follow, thus making biofilms impervious to anti-microbial therapies.
Medical Impact of Biofilms
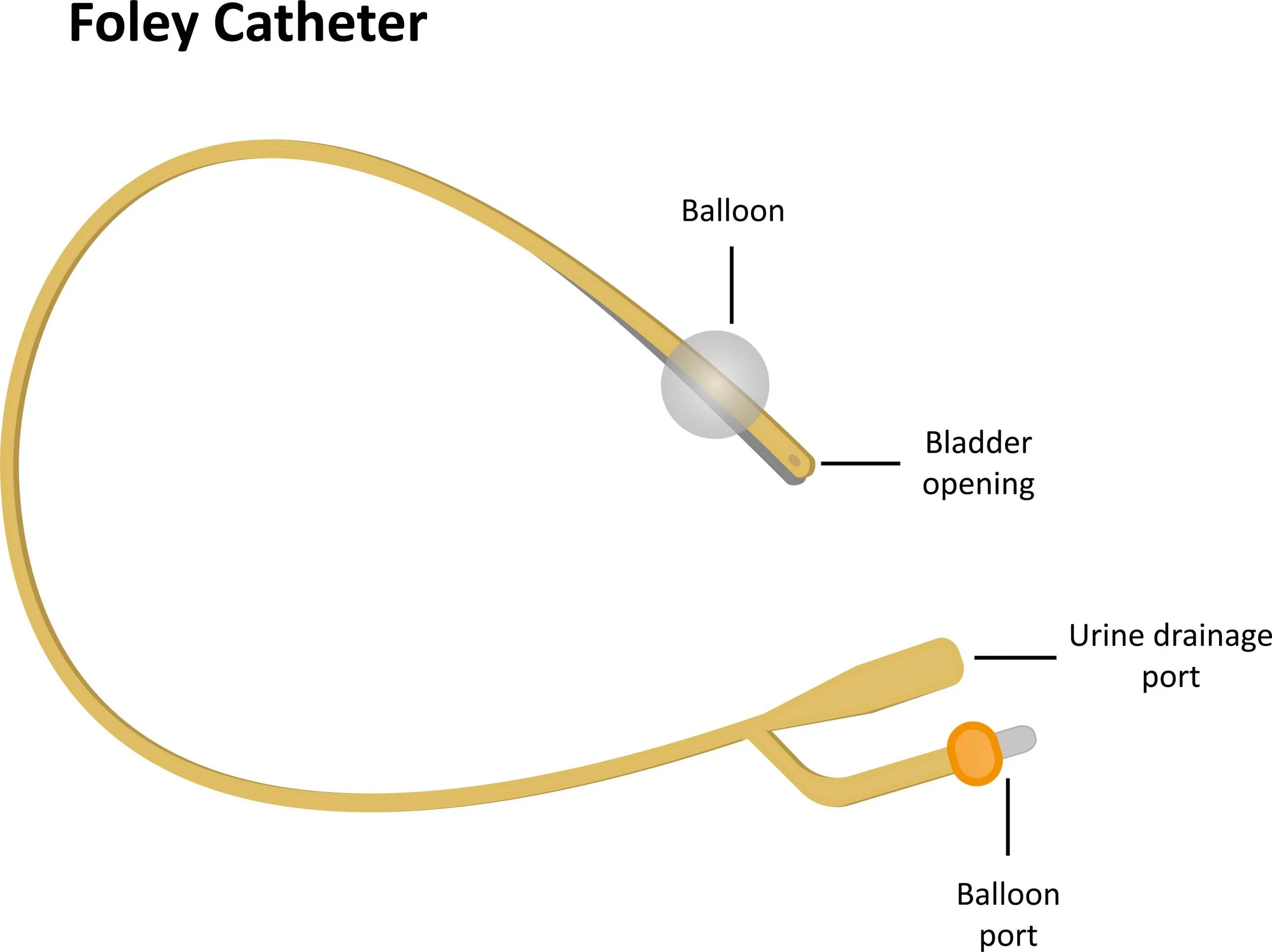
Biofilms can slow wound healing by causing prolonged inflammation, oxidative stress, and destruction of essential growth factors. They also form on medical devices, such as urinary catheters, where in some cases, mineral-rich biofilms trap bacteria and obstruct flow, creating serious infection risks.
Industrial Impact of Biofilms
In oil & gas industries, biofilms can cause macro-fouling and microbial-influenced corrosion (MIC). In pipelines, bacteria contribute to internal and external corrosion, resulting in multi-billion expenses for repairs and maintenance, annually.
Preventing Biofilms with IASIS Materials
IASIS has developed antimicrobial polymer fillers that can be incorporated into various materials and processed using standard methods including molding, extrusion, or coating. These modified surfaces are inhospitable to microorganisms, thus reducing biofilm formation.
High Touch Surfaces in Hospital and Clinical Settings
Multiple studies show that pathogens responsible for healthcare-associated infections (HAIs) frequently contaminate patient environments. This includes porous surfaces, such as curtains, as well as hard, non-porous surfaces like bed rails and medical equipment.
Contaminated surfaces act as reservoirs for pathogen transmission—either directly through patient contact or indirectly via healthcare workers’ hands and gloves. Even after disinfection with bleach, quaternary ammonium compounds (QAC), UV light, or hydrogen peroxide vapor, hospital surfaces can remain unsanitary. Copper surfaces, however, have been widely recognized for their ability to inhibit a broad range of microorganisms, including viruses.
Walls and floors represent the largest areas at risk for contamination in hospitals, clinics, nursing homes, daycare centers, and gyms, where pathogens pose a significant concern. IASIS composite surfaces help reduce microbial burden, thus providing protection healthcare and other high-contact environments.